CARTILAGE RESTORATION EXPERT
Damage to both the bone beneath the articular cartilage and the smooth, articular cartilage covering the ends of bones is referred to as an osteochondral lesion. Although they can occur in any joint, they are most frequently seen in the knee and ankle. This kind of damage usually arises from a direct hit to the joint. Ankle sprains and twisted knees are examples of this. It is unknown what specifically caused the lesions. Either a hereditary predisposition or aberrant bone growth in childhood could be the cause. The formation of the lesions has also been linked to inadequate blood flow to the affected area and repetitive stress.
An osteochondral lesion interferes with a joint's natural function in several ways. The damage creates a rough spot on the smooth joint surface which can cause pain and a feeling of “catching” during movement. This roughness triggers an inflammatory response in the body, which causes swelling, discomfort, and stiffness. The lesion weakens the support for the joint surface, which could lead to instability, because it affects the bone that lies beneath the cartilage. Additionally, the injury may aggravate bone nerve endings, causing pain signals to be sent even when the joint is not moving.
The damaged area may worsen with continued usage of the affected joint, resulting in persistent pain and potentially exacerbating the injury over time. Furthermore, the lesion may obstruct normal joint fluid flow, which typically promotes smooth mobility. These elements work together to cause pain, swelling, stiffness, and an overall sense that something is wrong with the joint. If neglected, these disorders may worsen over time and possibly cause early-onset arthritis in the afflicted joint.
Portland’s Top Osteochondral Lesion Surgeon
MACI PROCEDURE
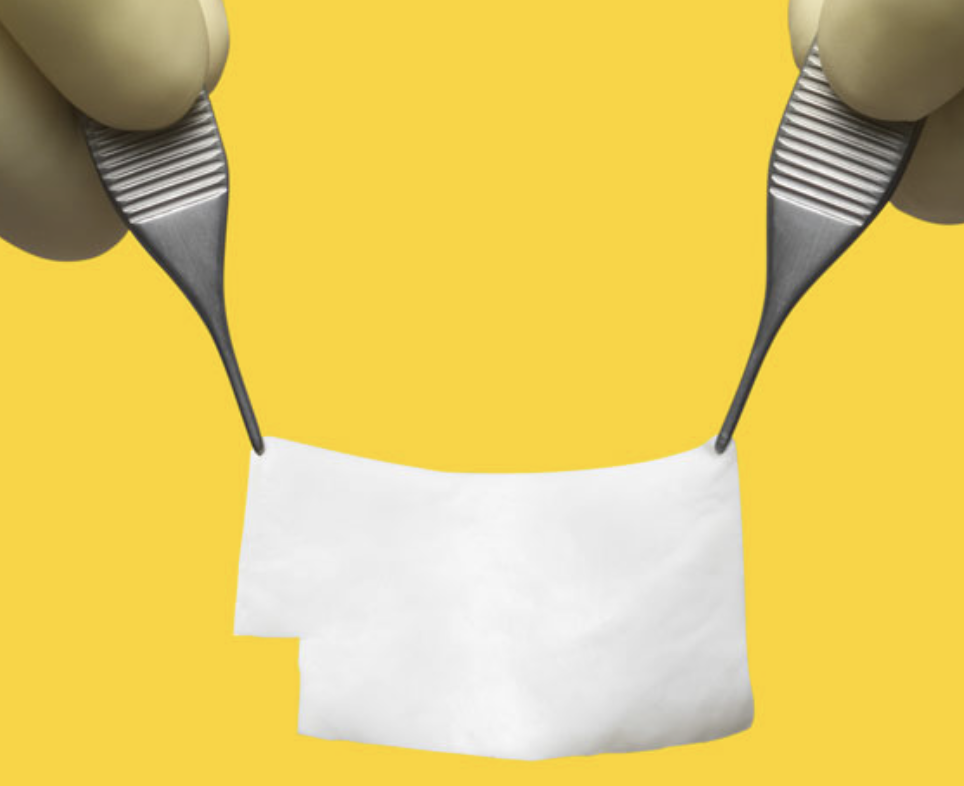
The MACI (Matrix-Induced Autologous Chondrocyte Implantation) procedure is a cutting-edge therapy that restores damaged joint cartilage. It is a two-step procedure that creates new cartilage using your own cells. In the first step, the surgeon takes a small sample of healthy cartilage from your joint. This sample is sent to a lab where your cartilage cells are extracted and grown on a special membrane. In the second step, the surgeon removes the damaged cartilage from your joint. They then implant the membrane with your newly grown cartilage cells into the area of damage. Over time, these cells proliferate and integrate with your existing cartilage, forming a new, healthy joint surface.
MACI is particularly useful for larger areas of cartilage damage. It seeks to lessen discomfort, enhance joint functionality, and maybe postpone or avoid the need for joint replacement surgery. Recovery typically involves physical therapy and a gradual return to activities over several months. This treatment offers a more customized approach to cartilage restoration by utilizing your own cells to restore your joint and has been recognized as a big advancement in the field of biologics.
Cartilage Transplant Surgeon Near You
OATS PROCEDURE
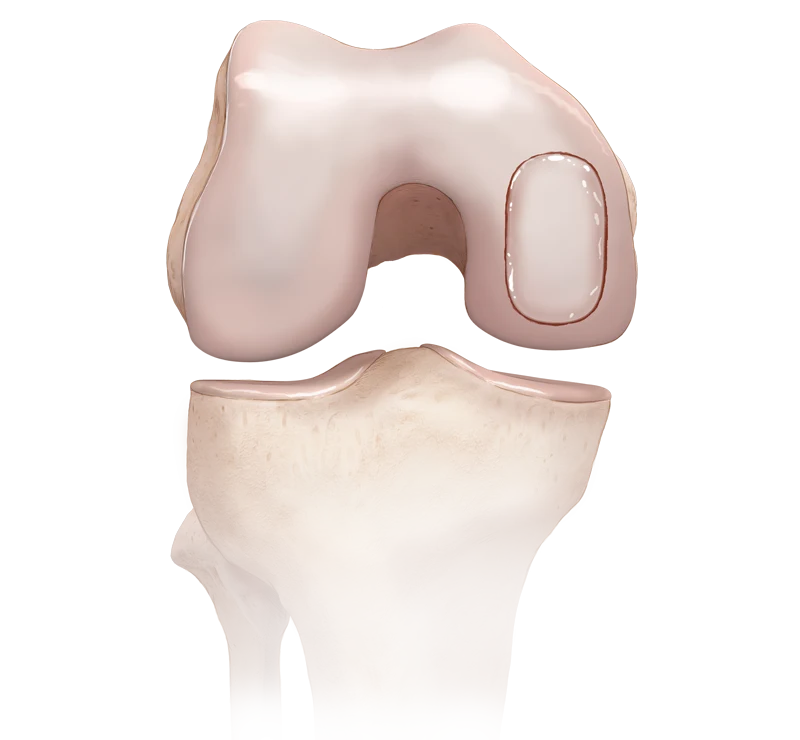
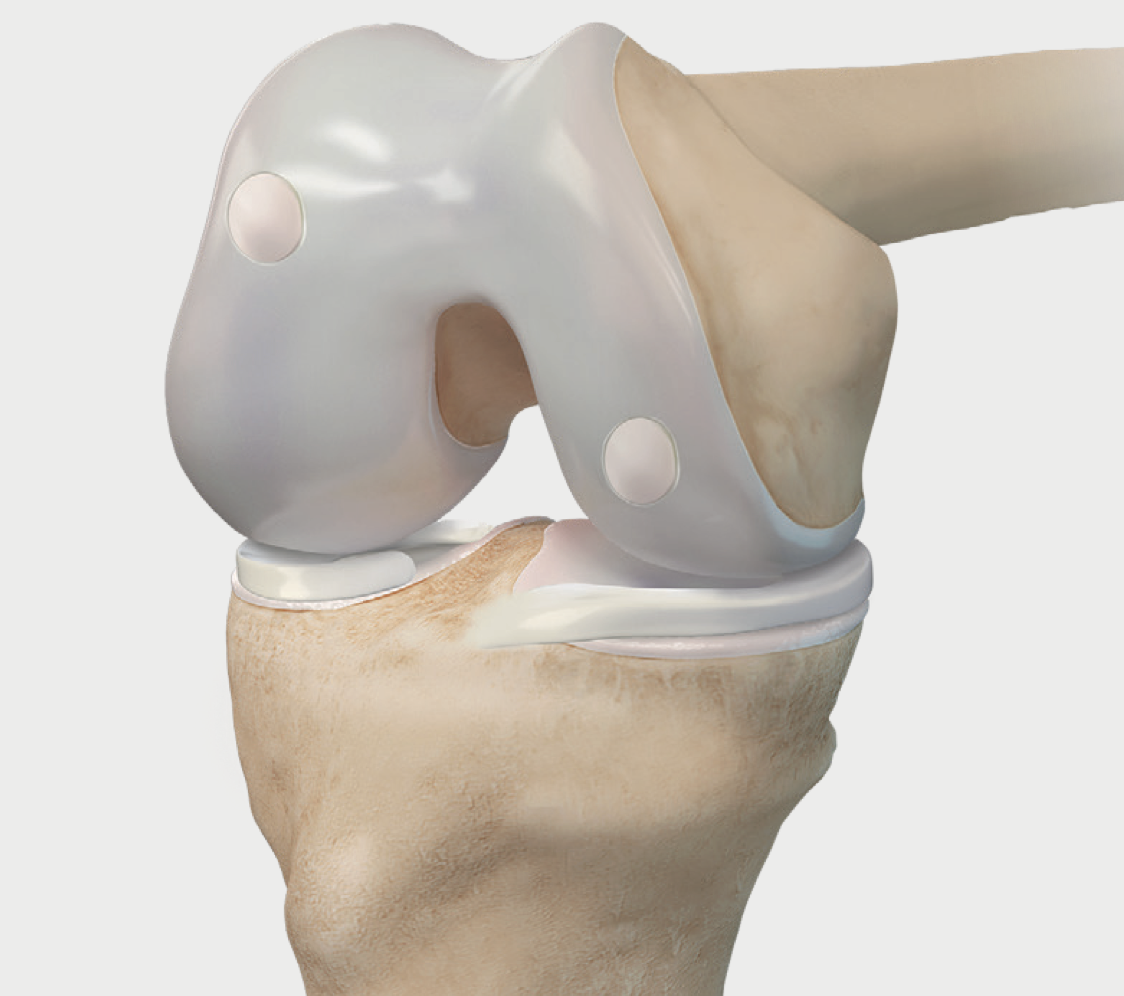
The OATS (Osteochondral Autograft Transfer System) procedure is a surgical technique primarily used to treat large, symptomatic lesions with a particular focus on knee injuries. This method aims to repair damaged cartilage by transferring healthy cartilage and bone from a non-weight-bearing area to the damaged site.
The OATS procedure is done under general anesthesia. After an arthroscopic examination of the injury, the surgeon will create a tiny hole in the damaged cartilage where the plug will be inserted. Next, a cartilage plug from the knee's healthy area will be removed and implanted into the hole. After an OATS procedure, the transferred cartilage will grow into the damaged cartilage, ultimately resolving the patient’s knee pain. One of the main advantages of OATS is that it uses the patient's own tissue, which reduces the risk of rejection and disease transmission. Recovery generally involves a period of non-weight bearing, followed by a gradual return to normal activities.
MICROFRACTURE EXPERT
Microfracture surgery is a minimally invasive arthroscopic procedure aimed at restoring small areas of damaged cartilage in the knee. The surgery begins with an arthroscopic examination to assess and stabilize the affected area by removing loose cartilage and creating a stable rim. The surgeon then creates small holes, or microfractures, in the subchondral bone beneath the defect to allow growth factors and stem cells from the bone marrow to reach the site and form a clot, which serves as the foundation for new tissue formation. This clot eventually develops into durable repair tissue. After surgery, patients typically follow a careful rehabilitation protocol, starting with protected weight bearing around six weeks to ensure proper healing. Microfracture is commonly used for smaller cartilage defects, usually under 2-4 cm², and is favored for its simplicity and effectiveness as a first-line treatment.
Complex Cartilage and Joint Preservation Q&A
FREQUENTLY ASKED QUESTIONS
What are articular cartilage conditions, and how do they affect the knee or other joints?
Articular cartilage conditions involve damage or degeneration of the smooth, cushion-like cartilage that covers the ends of bones in joints. This cartilage allows for smooth movement and absorbs shock. When damaged, it can cause pain, stiffness, swelling, and reduced joint function. Common conditions include osteoarthritis, chondromalacia (softening of the cartilage), and cartilage tears.
What are the most common symptoms of articular cartilage damage
Symptoms of articular cartilage damage typically include joint pain, swelling, stiffness, reduced range of motion, and a feeling of grinding or clicking in the joint. These symptoms can worsen with activity and may improve with rest but often progress over time.
What treatment options are available for articular cartilage conditions?
Treatment options vary based on the severity of the cartilage damage. Conservative treatments include physical therapy, medications to reduce pain and inflammation, and joint injections with corticosteroids or hyaluronic acid. Advanced treatments might involve regenerative medicine techniques like platelet-rich plasma (PRP) or stem cell therapy, which aim to stimulate cartilage repair. In severe cases, surgical options such as microfracture, osteochondral autograft transfer, or cartilage restoration procedures may be considered.
How effective are regenerative medicine treatments for articular cartilage damage
Regenerative medicine treatments, such as PRP and stem cell therapy, can be effective for stimulating cartilage repair and reducing symptoms of articular cartilage damage. PRP therapy uses concentrated platelets to promote healing, while stem cell therapy uses cells capable of developing into cartilage tissue. These treatments often provide pain relief, improved joint function, and potentially slow the progression of cartilage degeneration, though results can vary from patient to patient.
What is the expected recovery time and rehabilitation process after treatment for articular cartilage conditions?
Recovery time and rehabilitation depend on the treatment type and the extent of cartilage damage. Conservative treatments may involve a few weeks to months of physical therapy and activity modification. For surgical procedures or regenerative medicine treatments, recovery can take several months and typically includes a structured rehabilitation program to restore strength, flexibility, and joint function. Patients should follow their healthcare provider’s recommendations and attend follow-up appointments to ensure optimal recovery and prevent further injury.

Make an appointment:
Multnomah Orthopedic Clinic
5050 NE Hoyt Street, #626
Portland, Oregon 97213
T: 503.231.1426
F: 503.231.0316
multnomahortho.com
BOOK AN APPOINTMENT